KANSAS CITY, Mo. — Important news for Medicaid recipients in Missouri: Payments for several Medicaid programs will resume in a few days, potentially impacting vulnerable individuals in the state.
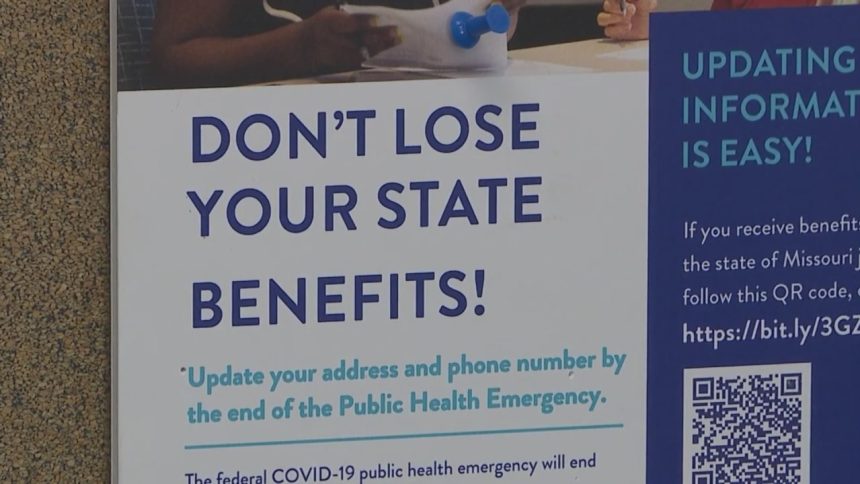
After a three-year freeze on Medicaid insurance payments due to COVID, Missouri is ending the suspension. KC CARE Health Center is urging patients to stay informed to prevent loss of coverage.
Missouri will reinstate payments for individuals covered by the CHIP, federal Children’s Health Insurance Program, Ticket to Work Program, and Spend Down Program.
“All of their premiums will resume,” said Emily Dreher, Manager of Eligibility and Enrollment at KC CARE health center.
KC CARE provides assistance with navigating Medicaid for community members.
Tens of thousands of low-income children, individuals with disabilities, the blind, and elderly people in Missouri are at risk of losing Medicaid coverage, according to KC CARE.
Individuals enrolled in the CHIP and Ticket to Work programs must pay May invoices to ensure coverage starting June 1st — and continue monthly payments.
If payment is not made, the individual may be removed from the program, KC CARE noted.
Those in the Spend Down Program must also begin paying their spend down amount to MO HealthNet in May for coverage starting June 1.
According to Dreher, monthly spend down amounts can range from $20 to $2,000, potentially creating financial burdens for participants.
“Failure to make payments could result in full-price medical bills or even denial of care, affecting access to treatment and prescription coverage,” Dreher warned.
Many individuals who rely on these programs may be unaware of the changes, which is why KC CARE is working to educate the community.
“There is assistance and free help available across the state,” Dreher emphasized.
Will Cann, a KC CARE patient, is currently examining his coverage options and expressed concern about potential barriers to care or increased costs.
“Discovering this at the doctor’s office would be distressing,” Cann stated. “It may hinder my ability to access necessary resources for daily living.”
Impacted individuals should receive a letter in the mail with payment instructions, according to Dreher.
For assistance with navigating this process, KC CARE Health Center offers support from staff members.
If you need to contact a Health Insurance Navigator at KC CARE, you can call (816) 777-2776 or email
Na********@kc****.org
.